If a crackle is heard in the knee joint during movement, this is the first sign of gonarthrosis. Conservative methods of traditional and alternative medicine will help prevent cartilage destruction and maintain normal motor function. Treatment should begin immediately - only in this case, rheumatologists give a favorable prognosis.
What is gonarthrosis?
A non-inflammatory, degenerative-dystrophic disease that affects the largest joint, the knee, is called gonarthrosis. A rather unusual medical definition, there is a simpler concept "popular" - "salt deposition". Although the clinical picture of joint gonarthrosis has little to do with an excess of calcified salts in the knee joint. They have no effect on pathology and are a side effect of impaired metabolism.
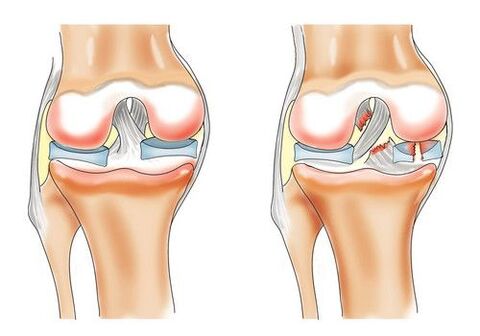
The development of gonarthrosis of the knee joint is facilitated by negative processes in the hyaline cartilage, mainly poor blood circulation in the small bone vessels. Lack of nutrients and oxygen carried by the lymph flow leads to the destruction of the outer layer of the knee cartilage.
In the early stages, the disease is extremely difficult to recognize. Deformation of the joint occurs slowly, until the hyaline cartilage of the glass is retracted in the process. The anatomical structure of the ligament has been modified. Turbulence occurs, the tissue thickens, becomes thin, cracks in all directions. The result of the pathology can be the complete disappearance of the cartilage, which leads to neoplasia in the bone tissue and irreversible curvature of the knee.
Classification of the disease
The International Classification of Diseases divides gonarthrosis into seven explanatory subheadings:
- Primary bilateral gonarthrosis. The diagnosis is most often made in women aged 70 to 74 years and in men aged 60 to 64 years. This puts the disease in the category of "elderly".
- Another primary gonarthrosis. Pathology of a knee joint, due to natural consumption or on the background of other diseases.
- Bilateral post-traumatic gonarthrosis. People of different age categories with severe foot injuries are affected.
- Other post-traumatic gonarthrosis. Unilateral, against the background of injuries and bruising of the limbs.
- Other secondary gonarthrosis is bilateral. They are the result of chronic bruising, fractures or dislocations, not completely cured. It is most often diagnosed in athletes who have heavy loads on both feet - soccer players, athletes, figure skaters.
- Other secondary gonarthrosis. Unilateral development of pathology related to the profession. For example, miners, metallurgists, fishermen.
- Gonarthrosis, unspecified. It is diagnosed with an unexplained etiology of the disease, after excluding age, occupational and genetic predisposition.
According to medical statistics, more than 10 million people of different age groups suffer from gonarthrosis of one type or another. Every year, about 3, 000 people with a definite diagnosis die.
Causes
Osteoarthritis of the knee joint develops due to impaired metabolism in the knee joint, which leads to a loss of softness and elasticity of the cartilage.
Destructive processes are caused by various reasons:
- Diseases of the thyroid gland, which violate the hormonal background;
- Reduced vascular permeability at the knee joint;
- genetic conditioning;
- natural aging;
- Knee injuries in the past or present, of various origins;
- Obesity (more than 20% of the norm), which puts a lot of pressure on the knee joint;
- Inflammatory diseases of the joints (polyarthritis, purulent arthrosis);
- Autoimmune diseases (rheumatoid arthritis);
- Specific infectious pathologies (syphilis, tuberculosis, encephalitis);
- Living in ecologically unfavorable areas, poor quality of food and water.
Rheumatologists also identify some additional reasons that lead to the development of gonarthrosis. Dysplasia in newborns. With this diagnosis, the node is consumed faster. Changes in the structure of collagen lead to disruption of proteins located in connective tissue.
Symptoms depending on the degree of gonarthrosis
It is difficult to diagnose the initial stage of knee osteoarthritis. Only a description of the symptoms by the patients themselves and external examinations by rheumatologists make it possible to create a clinical picture that varies with each degree of gonarthrosis progression:
- Grade I gonarthrosis.Traction pain in the knee, feeling of some stiffness, partial loss of sensation, difficulty in bending the leg, especially after prolonged immobility, inability to walk or run for a long time, the appearance of slight swelling. As a rule, the symptoms disappear after rest or simple anesthetics.
- Grade II gonarthrosis.At this stage, it is already possible to determine the pathology on an X-ray examination. The pain becomes stronger and appears after each physical activity. Discomfort can still be relieved with rest. In the morning it becomes more difficult to straighten the legs, it takes some time to restore motor function. Discomfort is complemented by frequent cramps in the calf, especially at night. A crackle is heard during the movement. Swelling of the knee joint is pronounced. There are obvious signs of limb deformity.
- Grade III gonarthrosis.There are irreversible changes in the knee joint. Cartilage abnormalities can be unmistakably determined on a radiograph. Knee pain becomes constant, acute. The foot stops bending at the knee. The patient can not walk without a cane or crutches. Swelling is important. The anatomical shape of the knee softens and takes on a solid appearance. There is a primary curvature of the spine.

diagnostic
To establish an accurate diagnosis, a combination of clinical manifestations of knee arthrosis and patient complaints is used. To clarify or rule out the causes of the disease, studies are conducted in different ways.
The standard diagnosis goes as follows:
- Making a medical history. History of concomitant diseases, genetic predisposition, past traumas and surgical interventions, professional activities, etc.
- External evaluation of musculoskeletal system deformity. Walking, posture, knee joint condition, leg curvature.
- General inspection. Palpation of the lower leg, thigh, injured ankle, determination of the localization of the disease.
- Laboratory tests. A general blood test gives evidence of the absence of an inflammatory process. If the process is present against the background of other diseases, then an increased rate of erythrocyte sedimentation will be found in the blood. The level of protein, globulin and fibrinogen will differ from the normative indicators. The biochemical composition will remain within the standard limits. If the course of the pathology is in the final stages, then a biopsy of the synovial fluid of the knee is done.
- Instrumental research. X-rays are the main and most common method for diagnosing suspected gonarthrosis. As a rule, a rheumatologist can easily determine changes in bone tissue structure from a photograph already at the beginning of stage 2 disease. The presence of lateral diseases and the causes of their occurrence are diagnosed with the help of the most modern and accurate equipment - MRI, CT, ultrasound, osteostintigraphy, thermography.

Treatment of gonarthrosis
Like all joint diseases, gonarthrosis requires systemic treatment, which is desirable to start with the onset of the first symptoms. In this case, the prognosis of therapy becomes favorable and guarantees the return to a normal lifestyle in a fairly short time.
Comprehensive treatment aims to eliminate the main signs of the disease:
- Discomfort, pain syndrome, and muscle tone;
- Improving the motor function of the knee joint;
- Stopping the process of cartilage destruction;
- Strengthening the connective muscles;
- Restoration of normal blood circulation to the knee joint.
medications
Anti-inflammatory drugs
They help to cope with pain, to relieve swelling caused by inflammation of muscle tissue.
Chondroprotectors
Regeneration and restoration of cartilage tissue is impossible without chondroprotectors. They are the main component of conservative treatment.
Vasodilators
They are used to improve the permeability of intra-articular blood vessels.
Hormonal drugs
Reduce the production of the hormone cortisone, to prevent the development of inflammatory processes.
Hyaluronic acid injections
Used to restore intra-articular synovial fluid. Because of this, friction between the articular parts is reduced, motor function is normalized, and cartilage tissue elasticity is restored.
Anti-enzymatic agents
They inhibit the activity of trypsin, thus preventing further destruction of the joint. Named in the complex.
Physiotherapy
Physiological treatments have been used successfully for decades to treat osteoarthritis of the knee. It can be as a stand-alone therapy, for prevention or during the rehabilitation period. Thus is an integrated approach to disease.
Most often, the following types of procedures are prescribed by a rheumatologist:
- Soothing electrophoresis;
- Ultrasound treatment;
- Magnetotherapy;
- Laser exposure;
- Paraffin applications;
- Mud treatment;
- Therapeutic exercises (exercise therapy);
- Manual therapy, massage with medicated ointments.
Surgery and prosthesis
If gonarthrosis is in an advanced stage, the knee joint and cartilage tissues are destroyed, it is impossible to do without a surgical operation. Otherwise, the person will remain disabled for life.
Modern medicine offers several ways to solve the problem:
- Arthrodesis. Complete removal of affected tissue and knee joint. The body is freed from the focus of the disease, but the motor function of the limbs is completely lost. Used extremely rarely, if the patient has additional joint disease.
- Arthroscopy. Destroyed hyaline cartilage is removed. The operation is less traumatic, has a short rehabilitation period. Indicated for patients whose progression has not affected the knee joint itself.
- Periarticular osteoma. A complex operation, the essence of which is the insertion of deformed bones and outgrowths, with subsequent attachment to the necessary anatomical structure.
- Endoprosthetics. The completely destroyed knee joint is removed and a titanium prosthesis is placed in its place. An effective method that allows you to forget about gonarthrosis forever. Requires careful preparation and long rehabilitation.
Traditional medicine
The use of folk recipes in combination with conservative treatment can relieve external symptoms (pain, swelling). Recipes based on laurel leaf, burdock root, St. John's wort, malt and hay have proven themselves well. They are used to make ointments, creams, tinctures and decoctions.
These plants have anti-inflammatory and analgesic properties. Requires regular and long-term use to achieve visible results.
Honey-based ointments and compresses, with the addition of alcohol or apple cider vinegar, relieve swelling well and have a calming effect on the affected tissues.
A nutritious mixture is made from lemon and garlic, which is taken orally, from a teaspoon each, after breakfast and dinner. Such a recipe has an overall strengthening effect on the body, increases the permeability of blood vessels and nourishes the joints with beneficial trace elements.
It should be remembered that home treatments do not remove the main problem - the pathological destruction of the knee joint.

diets
Dietary compliance is an integral part of complex treatment. Adjusting your diet will not only help control weight, but will also provide bones and joints with essential vitamins.
For a patient diagnosed with gonarthrosis, it is contraindicated:
- Fried, spicy, salty, pickled food;
- Fatty juices;
- Sweet pastries;
- Fruit, with high content of acidic enzymes;
- Alcoholic drink.
The menu should be supplemented with raw vegetables, fruits and herbs, low-fat dairy products, bone broth and dishes containing gelatin (jelly, jelly).
Additional Methods
For the treatment of gonarthrosis, it is necessary to undergo regular spa treatment, at least once a year, if possible more often. Hydrotherapy, mud therapy and manual therapy procedures are able to preserve the disease for a long time and prevent the destruction of the joint.
You will need the rest of your life to keep a sore knee in a stable condition. But it can become quite beneficial for the body as a whole. Review of nutrition, elimination of bad habits, playing sports, visits to resorts - quality of life can be significantly improved.
It should be remembered that self-medication, ignoring the primary symptoms and unbearable stress on the injured knee joint can very quickly turn a healthy person into a helpless disabled person.






























